Location
Consulting Hours
Monday – Thursday
9.30 am – 4.30 pm

When you’re born, you have a certain lifetime supply of eggs. The older you get, the more this supply slowly decreases in quality and quantity. The AMH blood test measures the mow many eggs you could potentially produce at any one particular stage in your life.
AMH test accuracy does come with some limitations, so please remember that the test isn’t 100% accurate — and it’s only one of many tools we use to gauge your fertility potential.
If your ovulation is irregular, or you’re not ovulating less at certain times, or not at all, it can impact your fertility. But it doesn’t mean pregnancy is impossible; you might just need medical intervention and management. There are three main types of ovulation problems.
When the luteal phase (the second half of the menstrual cycle after ovulation) is shorter than normal, it’s difficult for a fertilised egg to implant in the uterus.
When your ovulation is inconsistent or it happens at irregular intervals, it could be caused by hormonal imbalances or underlying health issues.
When you don’t ovulate at all, it could be due to hormonal imbalances, stress, excessive exercise, Polycystic Ovary Syndrome (PCOS), or other conditions.

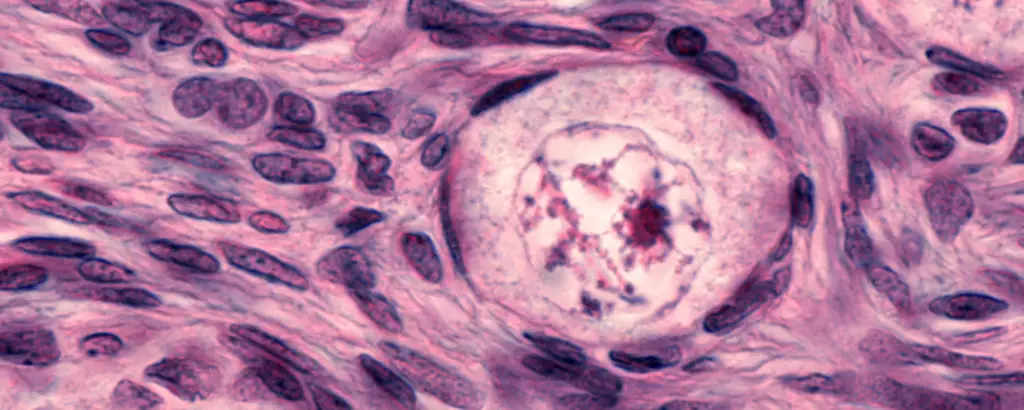
Fibroids and polyps are both non-cancerous growths that can occur in your uterus. But while fibroids are smooth muscle, polyps consist of the thin endometrial tissue that lines the uterus.
Fibroids can be detected through pelvic exams, ultrasounds, and other imaging techniques. Whole polyps are often diagnosed through hysteroscopy, where a thin tube with a camera is inserted into the uterus, so the doctor can visualise and remove the polyps.

Blocked tubes occur when there’s an obstruction in one or both of the tubes that connect your ovaries to your uterus. These tubes are essential for transporting eggs from the ovaries to the uterus and providing a pathway for sperm to fertilise the egg.
Blocked fallopian tubes are often diagnosed through a combination of medical history, physical exams, imaging tests, and minimally invasive procedures like a hysterosalpingography (HSG) — where a contrast dye is injected into your uterus, and X-rays are taken to visualise your fallopian tubes.
In cases of mild blockage, fertility medications or minimally invasive procedures like laparoscopy might be considered to improve tube function. For severe or irreparable blockages, assisted reproductive technologies such as IVF can bypass the fallopian tubes and increase the chances of pregnancy.
There are several potential causes, including:
When the tubes are blocked, the egg and sperm can’t meet, making natural conception difficult. And if an egg is fertilised but can’t travel through the blocked tube to reach your uterus, it can lead to an ectopic pregnancy, which is a serious medical condition.
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects people with ovaries. It is characterised by a combination of symptoms, including irregular menstrual cycles, excess androgen (male hormone) levels, and the presence of small cysts on your ovaries (though not everyone with PCOS will develop ovarian cysts).
The exact causes are still unclear, but it’s believed to involve a combination of genetic and environmental factors. Insulin resistance is also often associated with PCOS, which can lead to an overproduction of insulin, increasing your androgen levels and disrupting the normal menstrual cycle.
The symptoms can vary from woman to woman — but most often it’s irregular or infrequent menstrual, or even a lack of periods altogether. This makes it a leading cause of infertility
Diagnosis typically involves a combination of physical exams, medical history, and lab tests to measure your hormone levels, including androgens and insulin. An ultrasound may be used to visualise your ovaries and check for cysts (though not everyone with cysts will have PCOS).
Treatment depends on your individual symptoms and goals. Lifestyle changes, like maintaining a healthy weight through diet and exercise, can help manage symptoms. Medical options include birth control pills to regulate your menstruation, and clomiphene to induce ovulation.

It’s a chronic condition where tissue similar to the uterine lining grows outside your uterus, causing pain, menstrual irregularities, and potential blocked fallopian tubes.
Yes. Endometriosis can lead to pelvic scarring, tubal damage, and reduced egg quality, hindering natural conception. IVF bypasses these obstacles by directly fertilising eggs outside the body and transferring your resulting embryos into the uterus, increasing your chances of pregnancy.
Fertility issues aren’t limited to the female’s body, and it could be a problem with the male reproductive system, which might require a sperm count test — or a combination of both.
Here are the common male issues that male fertility testing is used to detect:
Causes include hormonal Imbalances like a low level of testosterone, enlarged veins within the scrotum (a condition called varicocele), certain infections can lead to temporary or permanent damage to the testicles, lifestyle factors like smoking, excessive alcohol consumption, drug use, and obesity, and genetic factors.
Insufficient motility, or the inability to move fast, is another possible reason for infertility in men. Causes include abnormalities in the structure of the sperm tail, hormonal imbalances, and varicocele.
Causes include genetic abnormalities, environmental factors like exposure to toxins and radiation, and the negative effects on sperm health of certain medications.
Most often, the issue can be determined with a sperm count test, which is the most common fertility test for men. But sometimes, sperm counts aren’t enough — additional tests are needed, like hormone (blood) tests, scrotal ultrasound and genetic testing.
Monday – Thursday
9.30 am – 4.30 pm